Integrating patient safety fundamentals in health sciences curriculum
 Patient safety principles and quality improvement methodology have become increasingly vital to healthcare organizations everywhere. The Institute of Medicine brought the importance of healthcare quality and safety into the spotlight with its report, To Err is Human: Building a Safer Health System.
Patient safety principles and quality improvement methodology have become increasingly vital to healthcare organizations everywhere. The Institute of Medicine brought the importance of healthcare quality and safety into the spotlight with its report, To Err is Human: Building a Safer Health System.
Accrediting organizations, payers (e.g., insurers, Medicare), and the public have all set high expectations for quality and safety in care delivery. In response, patient care organizations need knowledgeable staff applying quality and safety attitudes and methods on the frontlines of care. In other words, active engagement in quality and safety work is industry standard for all those working in healthcare.
Major leadership organizations — such as the Institute for Healthcare Improvement and World Health Organization (WHO, 2011) — have shared instructional curricular guides and resources in quality improvement and patient safety (QIPS). The Liaison Committee on Medical Education and the Accreditation Council for Graduate Medical Education have selected components of QIPS curricula for undergraduate and graduate medical education accreditation requirements, and providers must meet QIPS requirements as part of maintenance of board certification and state licensure renewals.
Fundamental attitudes, behaviors and habits key to QIPS activities are best developed when woven throughout the curriculum. Notably, learning would be greatly facilitated by students entering professional training with foundational QIPS knowledge and skills. High school courses exploring health and medical careers provide an opportunity for embedding terminology, methodology and approaches to QIPS. In addition to improving patient care and outcomes, the QIPS tools can apply to personal and professional goals.
This article describes examples of such an endeavor employed at the high school level. Billings Career Center, in Billings, Montana, embedded QIPS lessons in biomedical science courses to deepen students’ learning about careers in healthcare and prepare them for their role in ensuring patient safety.
Methodology
Principles of QIPS have been embedded into academic (knowledge-based) and clinical (patient care-oriented) courses at Billings Career Center over the past five years.
Patient safety principles are incorporated into courses that build on patient cases and care, such as:
- Principles of Biomedical Science
- Introduction to the Operating Room
Fundamental activities include:
- Proper patient identification using two patient identifiers,
- Hand hygiene
- Proper use of personal protective equipment
- Approaches key to clear team communication, written and verbal form
- Behaviors and ways to address populations and conditions with higher risk for error and harm
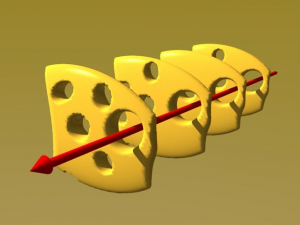 Consideration of medical errors begins with a writing assignment recalling experience with error or misunderstanding. The activity continues on to the Swiss cheese model for errors [Figure 1] and safety system design. Students learn basics of error recognition and reporting — see something, say something — including near misses, without harm. The National Patient Safety Foundation’s root cause analysis and action (RCAA) framework is used for learning from error with both non-medical and medical scenarios to identify system safety issues and actionable improvements.
Consideration of medical errors begins with a writing assignment recalling experience with error or misunderstanding. The activity continues on to the Swiss cheese model for errors [Figure 1] and safety system design. Students learn basics of error recognition and reporting — see something, say something — including near misses, without harm. The National Patient Safety Foundation’s root cause analysis and action (RCAA) framework is used for learning from error with both non-medical and medical scenarios to identify system safety issues and actionable improvements.
Results
Students write about a personal experience with error, guided with questions about:
- The action and reaction
- Why the reaction seemed appropriate at the time
- What happened next
- The chain of events resulting in error or “bad” outcome
One particularly poignant submission by an 11th grader dealt with an episode recalled from when she was in elementary school. The incident made a deep impression on her, with insights gained from time and reflection.
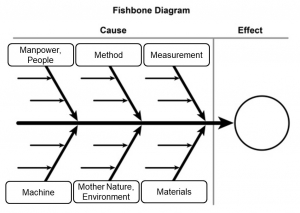
The RCAA begins with review of a non-medical, aviation incident, where students identify contributing factors to the fatal crash using the Ishikawa (fishbone) diagram structure [Figure 2]. Students gain experience with objective analysis of actions taken and choices made, and they reflect on observable changes implemented from the lessons learned.
Students then apply what they’ve learned to published medical cases on three types of clinical scenarios:
- Wrong patient, wrong procedure
- Retained foreign body
- Medication error
The analysis facilitates team and class discussions on factors contributing to errors and actions that can increase the opportunity to “get it right” and reduce error and harm.
Discussion
At what point students are ready for learning about quality improvement and patient safety? The question relates to timing in their respective curricula during which students are introduced into clinical experience with patient care. To that point, this author has spoken with numerous groups of high school juniors and seniors about their experience with health care and patient safety issues. A consistent finding is that while they don’t yet have patient care experience, they bring their own life experiences with health care systems, error and safety to the discussions.
Also consider teen mindset and attitudes about right and wrong. Lessons on errors need to address understanding versus judging, naming and blaming. As students develop their ability to understand other perspectives, small group discussions facilitate practice with this behavior.
Thirdly, for well-integrated patient safety lessons in the curriculum, students need to see relevance for the learning. Offering students an opportunity to select from topic or scenario options allows them to identify something meaningful to them.
Future opportunities
Three opportunities for further enhancements include:
- More team scenarios to practice communication and interpersonal interactions and support
- Increased focus on safety system design
- Integration of more simulated activities — clinical and non-clinical — into experiential learning in patient safety.
In conclusion, high school is not too early for teaching foundational principles and skills for improving patient safety and learning from error. These are fundamental characteristics on which postsecondary and professional education can build.
Constance Haan, M.D., M.S., M.A., is a cardiothoracic surgeon teaching at the Billings Career Center, growing biomedical course offerings, including clinical-based simulation education in the health sciences. She has been a medical educator for over 35 years, served as senior associate dean for educational affairs for UFCOM-J, and was clinical learning environment review site visitor for the ACGME. Email her.